Value-Based Care
Prepare for the New Paradigm

Value-based care services
Changing payment models from fee for service to value-based care - contracts that pay based on quality and total cost of care - are gaining momentum. In fact, CMS requires all Medicare patients to be in some form of a value-based model by 2030. This shift requires a different practice model, where providers must identify patients in need of care and provide proactive care that ensures patients stay healthy and avoid costly hospital stays. Failure to document and correctly code and bill for services results in missed incentive payments, lower risk scores, and, in down-side risk models, require re-payment to payers.
VBC relies heavily on documentation and claims data to drive risk and quality scores. Our coding, RCM , and staffing solutions enable your practice to reach patients and capture data on the initial claims submission rather than through time consuming retrospective reviews that frustrate staff and burn-out physicians. With Nath Healthcare, you can make the transition to value-based care and reach your goals of providing high-quality, cost-effective care.
Risk Adjustment Coding
Appropriate coding of ICD-10 codes drives risk scores and is foundational to VBC. Our coders provide prospective and retrospective reviews of patient medical records to identify conditions, ensure proper documentation, and report them on claims.
Quality Reporting
Quality reporting involves reviewing and educating providers on quality metrics. It is important to ensure that quality measures are accurately documented and closed. Quality codes should be reported on claims in order to close out care gaps and ensure that providers receive their incentive dollars.
Population Health
Population health involves managing payer portals, population health platforms and claims data in order to identify high-risk and high-cost patients, patients with care gaps, and those that have chronic conditions requiring follow up care. Traditional practice models do not have resources to manage population health systems and identify high-risk patients with care gaps that require care. Our virtual staff can perform these functions and perform tech-enabled patient outreach to get patients timely care.
Post-Discharge Management
Managing patients discharged from ER and inpatient setting is critical to managing readmissions and reducing costs. CMS requires contacting patients within 48 hours of discharge and a face to face encounter within 14 days for transitions of care. Traditional practice models do not have resources to monitor discharge notices and conduct the requisite patient outreach. With our virtual staff you can now timely identify the patients and get them scheduled to see providers increasing practice revenues and reducing cost of care.
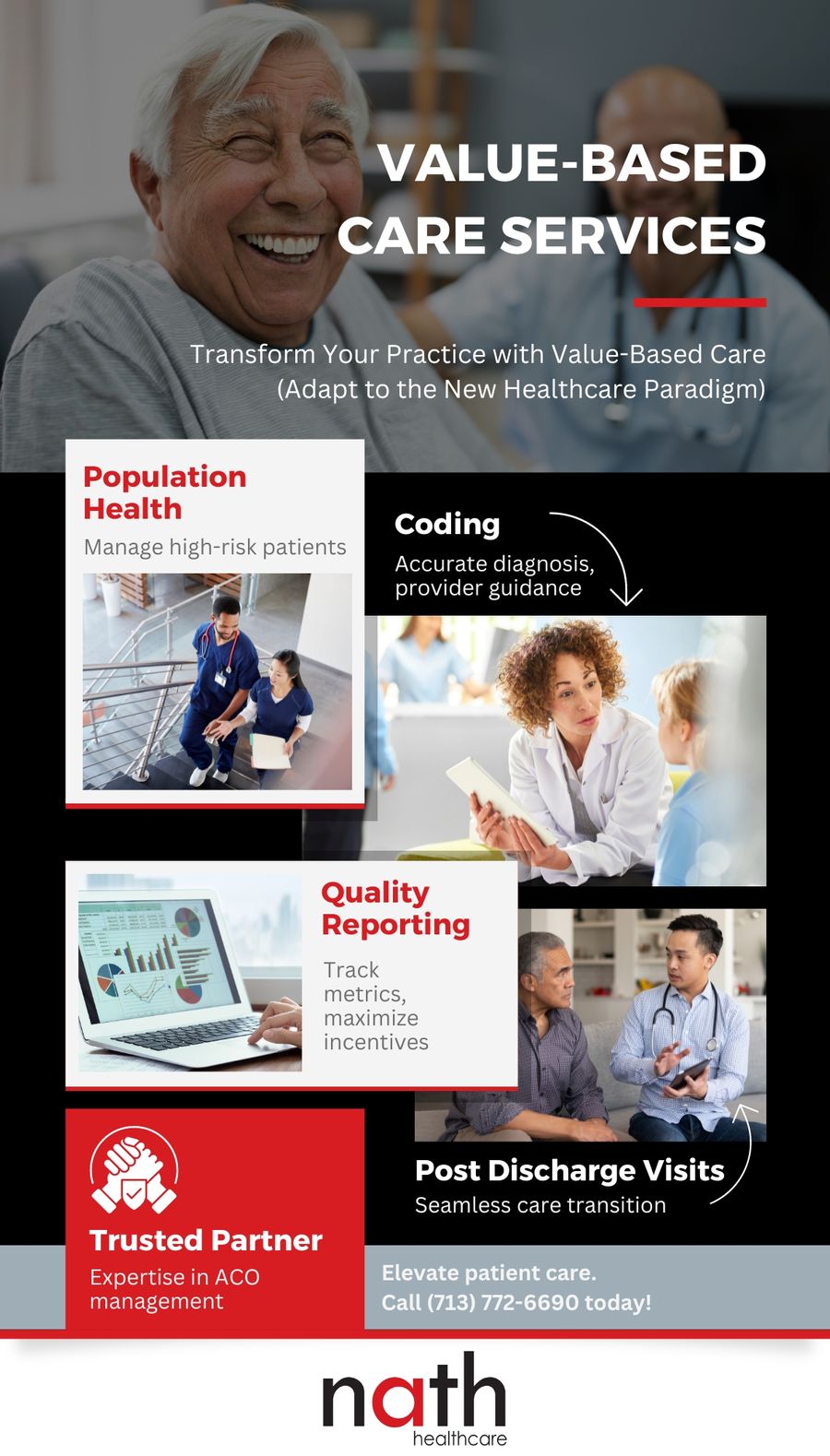

Why choose us
We have first-hand experiencing managing ACOs (Medicare Accountable Care Organizations) and appreciate the complexities inherent in better population health management, improving the patient experience and lowering cost of care, all while giving care teams a better work-life balance and greater professional satisfaction. While delivering on the quadruple aim is not easy we have the ability and motivation to win.
We are confident in our ability to deliver results and seek opportunities to partner with healthcare providers to take financial risk, including acquiring practices where appropriate.
